2406 Blue Ridge Road, Suite 190, Raleigh, NC 27607
(919) 594-1198
Fax (919) 882-8155
WEEKDAYS:
7:00am - 6:00pm
Contact Us
HOME / About Us
I agree to terms & conditions provided by the company. By providing my phone number, I agree to receive text messages from the business.
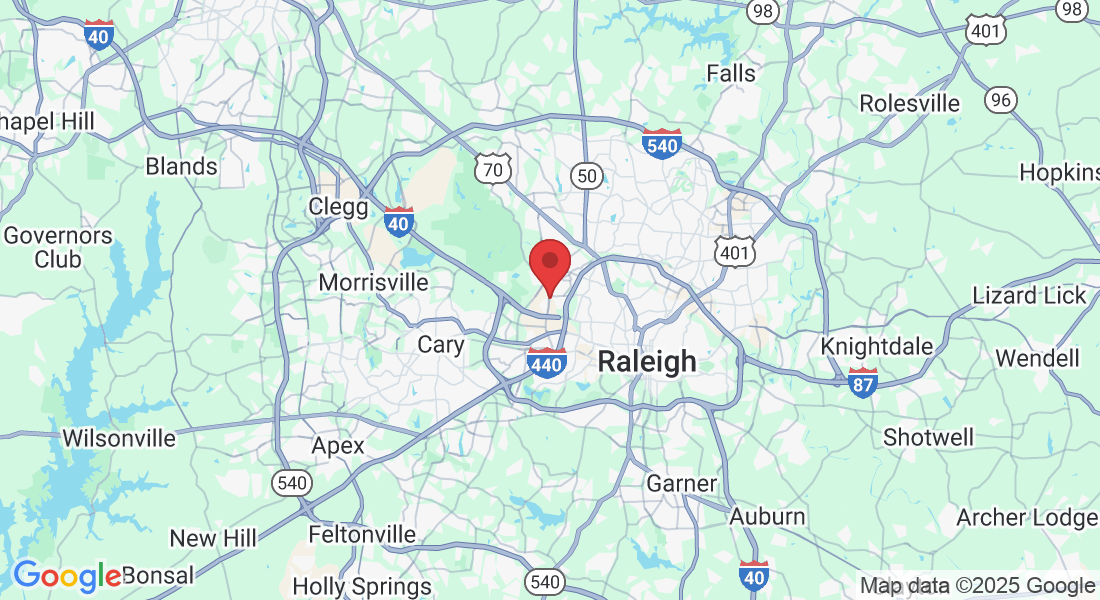
📍 Clinic Location
North Carolina Physical Therapy
2406 Blue Ridge Road, Suite 190
Raleigh, NC 27607
📞 Call or Text Us
(919) 594-1198
(919) 886-2652
📧 Email Us
📠 Fax Us
(919) 882-8155
🕒 Clinic Hours
Monday – Friday: 7:00am - 6:00pm
Need Directions?

2406 Blue Ridge Road, Suite 190, Raleigh, NC 27607
(919) 594-1198
(919) 882-8155
© 2025 | Privacy Policy